Associations of 24-Hour Urinary Sodium and Potassium Excretion with Cardiac Biomarkers: The Maastricht Study
Remy J H Martens, The Journal of Nutrition, Volume 150, Issue 6, June 2020, Pages 1413–1424,
Background
It is a matter of debate whether sodium and potassium intake are associated with heart disease. Further, the mechanisms underlying associations of sodium and potassium intake with cardiac events, if any, are not fully understood.
Objectives
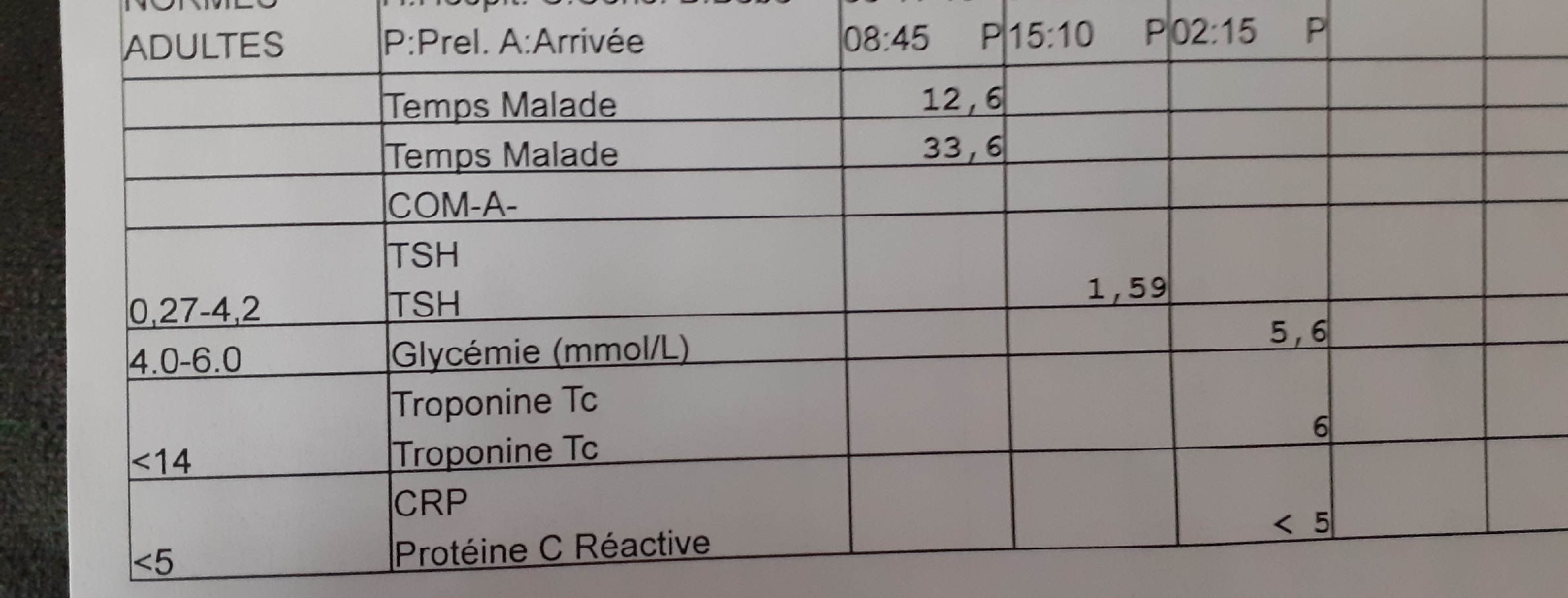
We examined cross-sectional associations of 24-h urinary sodium excretion (UNaE) and potassium excretion (UKE), as estimates of their intakes, with high-sensitivity cardiac troponins T (hs-cTnT) and I (hs-cTnI), and N-terminal pro-B-type natriuretic peptide (NT-proBNP), which are markers of cardiomyocyte injury and cardiac dysfunction.
Methods
We included 2961 participants from the population-based Maastricht Study (mean ± SD age 59.8 ± 8.2 y, 51.9% men), who completed the baseline survey between November 2010 and September 2013. Associations were examined with restricted cubic spline linear regression analyses and ordinary linear regression analyses, adjusted for demographics, lifestyle, and cardiovascular disease (CVD) risk factors.
Results
Median [IQR] 24-h UNaE and UKE were 3.7 [2.8–4.7] g/24 h and 3.0 [2.4–3.6] g/24 h, respectively. After adjustment for potential confounders, 24-h UNaE was not associated with hs-cTnT, hs-cTnI, and NT-proBNP concentrations. In contrast, after adjustment for potential confounders, lower 24-h UKE was nonlinearly associated with higher hs-cTnT and NT-proBNP. For example, as compared with the third/median quintile of 24-h UKE (range: 2.8–3.2 g/24 h), participants in the first quintile (range: 0.5–2.3 g/24 h) had 1.05 (95% CI: 0.99, 1.11) times higher hs-cTnT and 1.14 (95% CI: 1.03, 1.26) times higher NT-proBNP. Associations were similar after further adjustment for estimated glomerular filtration rate, albuminuria, blood pressure, and serum potassium.
Conclusions
Twenty-four-hour UNaE was not associated with the studied cardiac biomarkers. In contrast, lower 24-h UKE was nonlinearly associated with higher hs-cTnT and NT-proBNP. This finding supports recommendations to increase potassium intake in the general population. In addition, it suggests that cardiac dysfunction and/or cardiomyocyte injury may underlie previously reported associations of lower potassium intake with CVD mortality.