Frequency of osteoarthritis in athletes participating in summer olympics in Rio 2016
A. Merritt Osteoarthritis and Cartilage VOLUME 28, SUPPLEMENT 1, S297-S298, APRIL 01, 2020
Purpose: To describe the frequency and severity of osteoarthritis (OA) in athletes participating in the Rio de Janeiro 2016 Summer Olympic Games as assessed using magnetic resonance imaging (MRI).
Methods: The current study is based on a retrospective analysis of all MRIs of athletes who underwent MRI at the centralized core imaging facility of the International Olympic Commission (IOC) during the Rio 2016 Summer Olympics. Athletes were imaged for a multitude of reasons but had MRI mainly for suspected structural damage following acute trauma or non-traumatic pain. Patient demographics were collected from the IOC athlete database and imaging data were collected from the Radiological Information System and Picture Archiving Communications System of the Olympics medical staff. MRI imaging was performed within the Olympic Village through the official IOC clinic, using 3T Discovery MR750w and 1.5T Optima 450 MRw MR systems (both GE Healthcare, Brazil). All MRIs were reviewed for presence and severity of OA features primarily by one radiologist adjudicated by a second experienced radiologist. Scoring of MRI abnormalities was blinded to the initial reports. The MRIs of six anatomical regions / articulations were included and assessed retrospectively: shoulders, elbows, wrists, hips, knees and ankles. Osteophytes were scored as present (=definite osteophyte) or absent, and cartilage damage was scored form 0 to 3 according to a modified Outerbridge scale. These data were grouped into different severity grades based on the following classification: mild OA=presence of definite osteophyte and cartilage damage grade 1 (i.e. defect not exceeding 50% depth); moderate OA=presence of osteophyte and cartilage damage grade 2 (i.e. more than 50% in depth but no full thickness damage; severe (i.e. presence of osteophyte and cartilage damage grade 3 (i.e. any full thickness damage). Proportion of OA was tabulated for the entire sample, and grouped into sports categories (athletics, ball sports, other). In addition, results were categorized according to age strata (<25; 25-30; and >30 years of age) and by sex.
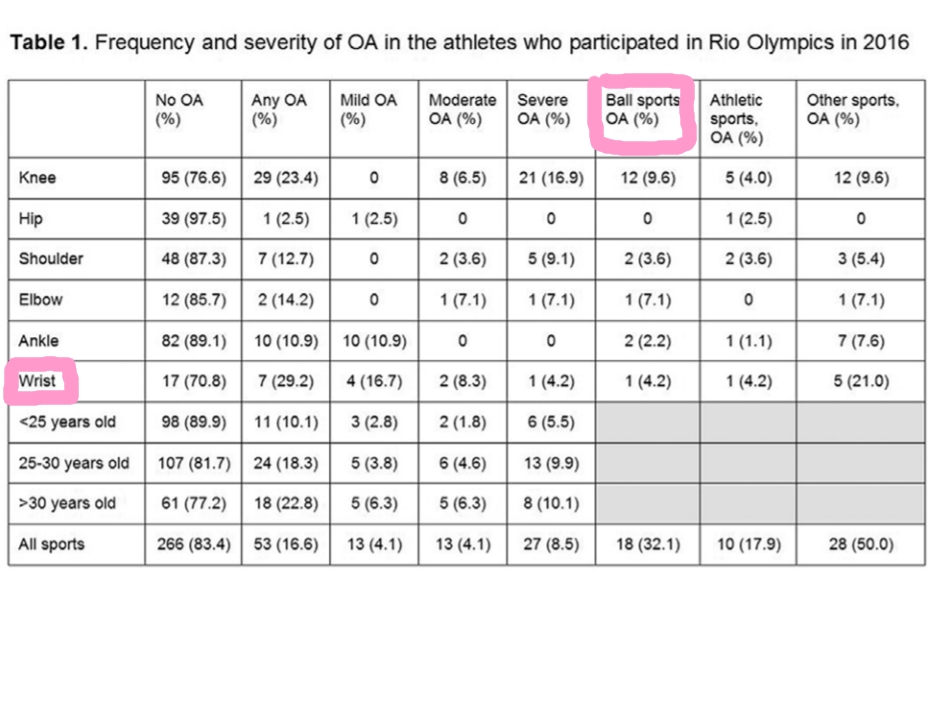
Results: A total of 11,274 athletes participated in the Games. 319 (2.8%) athletes underwent MRI of one or more of the mentioned anatomic locations. 160 (50.2%) were female, 109 (34.2%) were < 25 years, 131 (41.1%) between 25 and 30, and 79 (24.8%) > 30 years of age. 53 (16.6%) of the athletes that had MRI examinations were found to have underlying OA with 13 (4.1%) having mild OA, 13 (4.1%) moderate, and 27 (8.5%) severe OA. Within the category of ball sports knees were found to have the highest prevalence of OA with 9.6%. Within the categories of athletics and other sports, wrists were found to have the highest prevalence of OA at 4.2% and 21.0%, respectively. Of all athletes younger than 25 years 11 (10.1%), of those between 25-30 years of age 24 (18.3%) and of those older 30 years of age 18 (22.8%) were found to have OA. Of all athletes with OA the wrist (29.2%) and the knee (23.3%) were most commonly affected. (Table 1).
Conclusions: In this highly selected sample of athletes that underwent MRI of one of 6 major joints at the Rio Summer Olympics a frequency of 16.6% of any osteoarthritis on MRI was observed. Severe OA was more common than low or moderate OA possibly reflecting that these athletes are more likely to receive an MRI during competition than others. Of athletes with OA, the wrist was the most likely anatomic location to be involved. Frequency of OA was higher in athletes of 30 years or older.