Circulating Omega-3 Fatty Acids and Incident Adverse Events in Patients With Acute Myocardial Infarction
Iolanda Lázaro, J Am Coll Cardiol. 2020 Oct, 76 (18) 2089–2097
Background
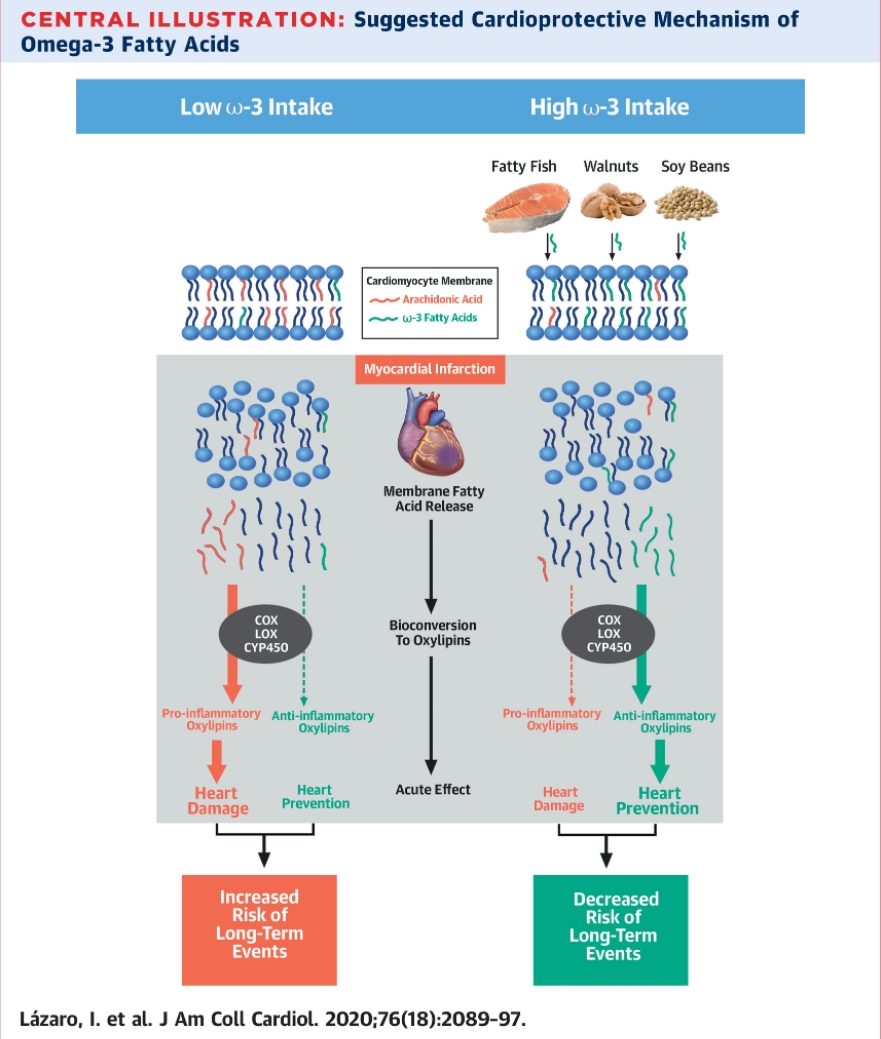
Dietary omega-3 eicosapentaenoic acid (EPA) has multiple cardioprotective properties. The proportion of EPA in serum phosphatidylcholine (PC) mirrors dietary EPA intake during previous weeks. Circulating EPA in ST-segment elevation myocardial infarction (STEMI) relates to smaller infarct size and preserved long-term ventricular function.
Objectives
The authors investigated whether serum-PC EPA (proxy for marine omega-3 consumption) levels at the time of STEMI were associated with a lower incidence of major adverse cardiovascular events (MACE), all-cause mortality, and readmission for cardiovascular (CV) causes at 3 years’ follow-up. We also explored the association of alpha-linolenic acid (ALA, proxy for vegetable omega-3 intake) with all-cause mortality and MACE.
Methods
The authors prospectively included 944 consecutive patients with STEMI (mean age 61 years, 209 women) undergoing primary percutaneous coronary intervention. We determined serum-PC fatty acids with gas chromatography.
Results
During follow-up, 211 patients had MACE, 108 died, and 130 were readmitted for CV causes. A Cox proportional hazards model adjusted for known clinical predictors showed that serum-PC EPA at the time of STEMI was inversely associated with both incident MACE and CV readmission (hazard ratio [HR]: 0.76; 95% confidence interval [CI]: 0.62 to 0.94, and HR: 0.74; 95% CI: 0.58 to 0.95, respectively, for a 1-standard deviation [SD] increase). Serum-PC ALA was inversely related to all-cause mortality (HR: 0.65; 95% CI: 0.44 to 0.96, for a 1-SD increase).
Conclusions
Elevated serum-PC EPA and ALA levels at the time of STEMI were associated with a lower risk of clinical adverse events. Consumption of foods rich in these fatty acids might improve the prognosis of STEMI.