Long-term effects of vitamin d supplementation and maintaining vitamin d sufficiency on knee osteoarthritis over 5 years
B. Antony Osteoarthritis and Cartilage VOLUME 26, SUPPLEMENT 1, S302-S303, APRIL 01, 2018
Purpose: Epidemiological studies suggest that vitamin D deficiency is associated with knee symptom and structural progression of knee osteoarthritis (OA). However, randomised controlled trials (RCTs) failed to demonstrate a significant effect of vitamin D supplementation on OA, probably due to selecting OA participants with and without vitamin D deficiency, short duration of the studies and a large proportion of participants in the placebo group reaching vitamin D sufficiency (61.3% of patients in the placebo group achieved a serum 25-hydroxyvitamin D [25(OH)D] level of > 60 nmol/l at 3 months of a clinical trial).
We conducted the Vitamin D Effect on Osteoarthritis (VIDEO) clinical trial by selecting knee OA participants with vitamin D insufficiency and reported that there was no significant effect of vitamin D supplementation over 2 years on cartilage volume loss and knee pain assessed using the WOMAC scale. However, there was a significant reduction in knee pain evaluated by VAS knee pain scale, an improvement in physical function and a decrease in joint effusion-synovitis volume and bone marrow oedema compared to the placebo group.
We aimed to describe the effect of vitamin D supplementation for 2 years on knee symptoms compared to placebo after 3 years of cessation of treatment, and to examine whether those maintaining sufficient serum vitamin D levels over 5 years had reduced knee symptoms compared with those who did not maintain adequate vitamin D levels over 5 years in patients with knee OA.
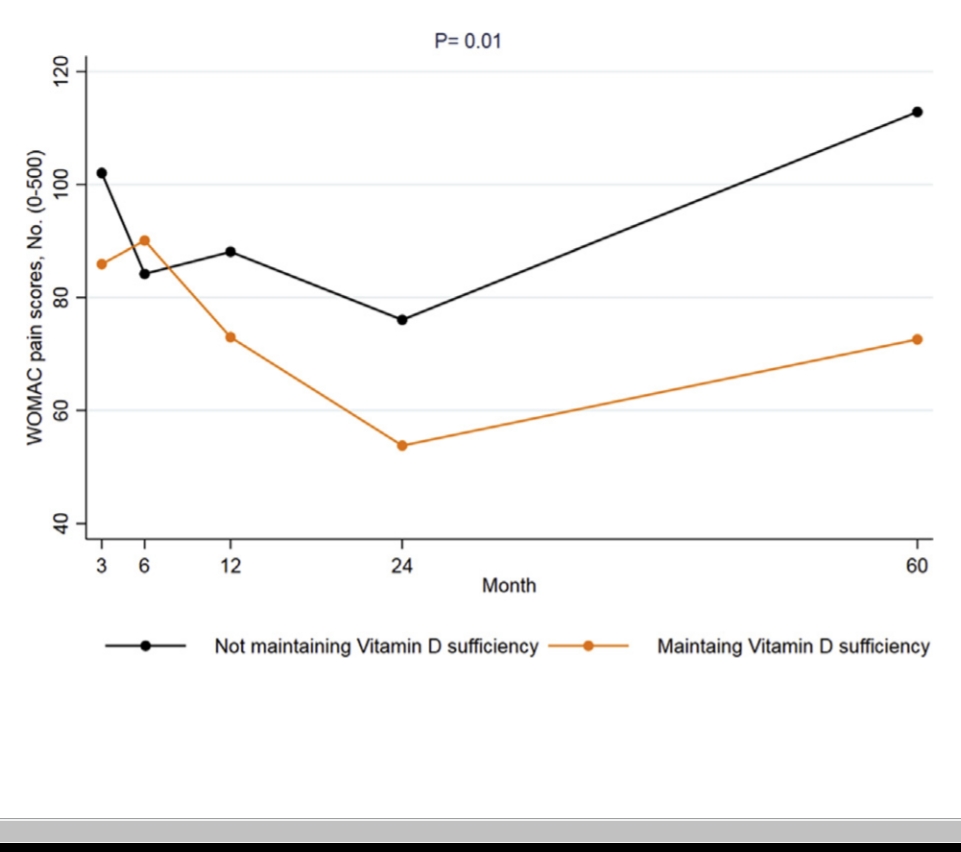
Methods: Participants with symptomatic knee OA and low 25(OH)D (12.5-60 nmol/l) were enrolled in the VIDEO clinical trial. Participants were randomly assigned to receive monthly treatment with oral vitamin D3 (50,000 IU; n = 209) or an identical placebo (n = 204) for 2 years. 172 participants who enrolled in the study from Hobart were followed up after 3 years (5 years from baseline) of the cessation of the treatment to assess knee symptoms and vitamin D levels. Participants with serum 25(OH)D measurements at month 0, 3, 24 and 60 and were included in the post-hoc analyses. The incidence of total knee replacement was recorded and they were excluded from the symptom analyses. Participants were classified as maintaining sufficient vitamin D group if they maintained serum 25(OH)D >50 nmol/l at month 3, 24 and 60 (n = 79), and not maintaining sufficient vitamin D group (25[OH]D ≤50 nmol/l at month 3, 24 and 60, n = 62). Knee symptoms were assessed at baseline, 3, 6, 12, 24 and 60 months using Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).
Results: The level of 25(OH)D dropped in the vitamin D group (from 87.0 nmol/l to 53.3 nmol/l) over 3 years after the cessation of the treatment. Placebo group slightly increased the vitamin D level (53.3 nmol/l to 61.7 nmol/l) over 3 years. Knee pain increased from the end of the study (2nd year) to 5 years of follow-up in the treatment (81.8 to 91.7) and placebo (75.8 to 101.1) groups. 16.7% of the participants in vitamin D and 18.5% of the participants in placebo group underwent total knee replacement surgery. There were no significant differences in WOMAC pain, stiffness or dysfunction scores and total knee replacement surgery rates or change in symptom between Vitamin D and placebo groups after 3 years of cessation of the supplementation.
However, participants who maintained adequate vitamin D levels over 5 years had significantly less WOMAC knee pain (β: −38.4, 95% CI: −69.2, −7.7) and physical dysfunction (β: −98.5, 95% CI: −193.8, −3.1) than participants with vitamin D deficiency over 5 years in multivariable analyses after adjusting for age, sex and BMI.
Conclusions: Vitamin D supplementation over 2 years did not result in significant differences in change in knee symptom score over 5 years compared to placebo. However, knee OA patients maintaining sufficient serum vitamin D levels over long-term had more improvement in knee pain and physical function than those who did not maintain adequate vitamin D levels, suggesting a beneficial effect of maintaining sufficient serum vitamin D for knee OA.