Vitamin K antagonist usage is associated with increased incidence and progression of osteoarthritis
C.G. Boer Osteoarthritis and Cartilage VOLUME 28, SUPPLEMENT 1, S405, APRIL 01, 2020
Purpose: Vitamin K has been hypothesized to play a role in osteoarthritis(OA) pathogenesis through its effects on several vitamin K-dependent bone and cartilage proteins, and therefore may represent a modifiable risk factor. Vitamin K antagonists (VKA) such as warfarin and acenocoumarol inhibit the vitamin K dependent blood coagulation for which they are prescribed. However, they potentially also inhibit the functioning of other vitamin K dependent proteins such as Matrix Gla Protein (MGP), an essential inhibitor of calcification in cartilage. A genetic variant in MGP has been associated with an increased risk for osteoarthritis and decreased MGP expression. Therefore, we investigated the effect of acenocoumarol usage, a vitamin K antagonist, on progression of radiographic OA in 5,218 participants of the Rotterdam Study cohort. Furthermore, we examined the effect of functional genetic variants of the MGP gene and VKORC1, a rate limiting enzyme in the Vitamin K metabolism.
Methods: We used data from in total 5,218 elderly participants that were not using acenocoumarol at baseline, from two prospective population-based cohorts within the Rotterdam Study (RS), RSI and RSII. Radiographs of the knees and hips were obtained at baseline and after 10 years of follow up. Any increase in KL-score was defined as overall progression (incidence and progression). Information on acenocoumarol usage and duration of usage during follow-up was collected from computerized pharmacy databases. The risk of osteoarthritis progression in acenocoumarol users was compared to that of non-users. Adjusted logistic regression analyses with generalized estimating equations (GEE) were used to calculate Odds Ratios (OR) and 95% Confidence Intervals (CI) for each joint group separately after adjusting for confounding variables and risk factors: age, sex, BMI, follow-up time, KL-score at baseline, lower limb disability and other medication usage.
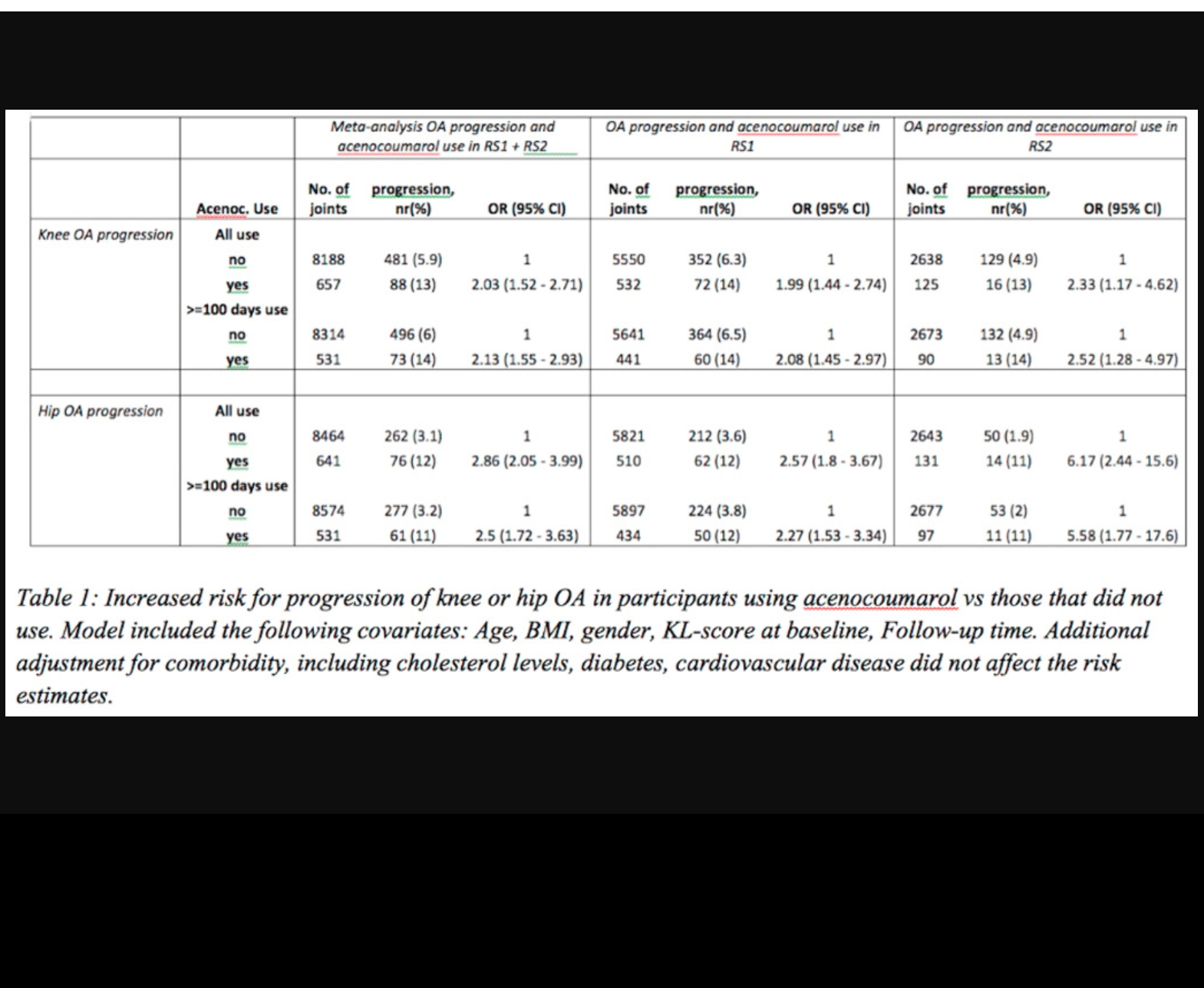
Results: Acenocoumarol usage was associated with a more than two-fold increased risk for OA progression and incidence (OR=2.3, 95%CI=1.9-2.9, p=6.7*10-16). This effect was observed in both knee (OR=1.9, 95%CI=1.5-2.5) and hip osteoarthritis (OR=3.0, 95%CI=2.2-4.2) separately. The increased risk was consistent in participants using acenocoumarol for >100 days. To account for potential confounding by indication, we also studied the effect of anti-platelet medication, as indications for this medication partly overlaps with that of acenocoumarol. We did not observe an effect on OA progression in the anti-platelet user group (n=976, OR=1.02, 95%CI=0.85-1.23, p=0.83). We also examined the effect of MGP and VKORC1 single nucleotide variants on this association. This as maintenance dosages of VKAs have been shown to be highly dependent on VKORC1 genetic variants effecting VKORC1 expression, and altered VKORC1 expression can also affect MGP function. We observed that the increased OA progression risk in acenocoumarol users is largely dependent on the MGP OA risk allele and VKORC1 high expression haplotype. Carriers of the MGP OA risk allele, with high VKORC1(BB) expression haplotype and using acenocoumarol had an almost four-fold increased risk of OA progression (OR=3.7, 95%CI=2.6-5.5, p=9.3*10-12) compared to non-users of that group (OR=1.5, 95%CI=0.8-2.8, p=0.18).
Conclusions: Vitamin K antagonist usage was associated with a more than two-fold higher risk of OA progression in both hip and knee joints. This risk increased to an almost four-fold higher risk when Vitamin K antagonist users were also carriers of the MGP OA risk variant and had the VKORC1 high expression haplotype. Thus Vitamin K antagonists, possibly through the inhibition of MGP function, modify the development and progression of OA. highlighting the importance of vitamin K and vitamin K Gla proteins, including MGP, in the pathogenesis of OA. Given that there are as yet no treatment options for preventing OA onset or progression, these data provide strong rationale for a properly powered randomized clinical trial of vitamin K in an appropriate patient population, such as those with insufficient vitamin K levels and/or MGP risk allele carriers. Additionally, these data lend support to the future possibility of genetic screening to identify individuals at high risk of OA incidence and progression.