Joint association of physical activity and body mass index with cardiovascular risk: a nationwide population-based cross-sectional study
Pedro L Valenzuela, European Journal of Preventive Cardiology, 22 January 2021
The prevalence of overweight and obesity has reached pandemic proportions, and people with these conditions present with an increased cardiometabolic risk.1 Some evidence suggests, however, that a high cardiorespiratory fitness (CRF) might mitigate the detrimental effects of excess body weight on cardiometabolic health, termed the ‘fat but fit’ paradox.2 For instance, a recent meta-analysis concluded that although both overweight/obesity and a low CRF can increase the risk of mortality from cardiovascular diseases (CVD), low CRF is actually a stronger predictor.3 Thus, it has been proposed that health policies should focus on physical activity (PA)-based interventions aimed at improving CRF rather than—or at least as much as—on weight loss strategies,3 although some controversy remains.2
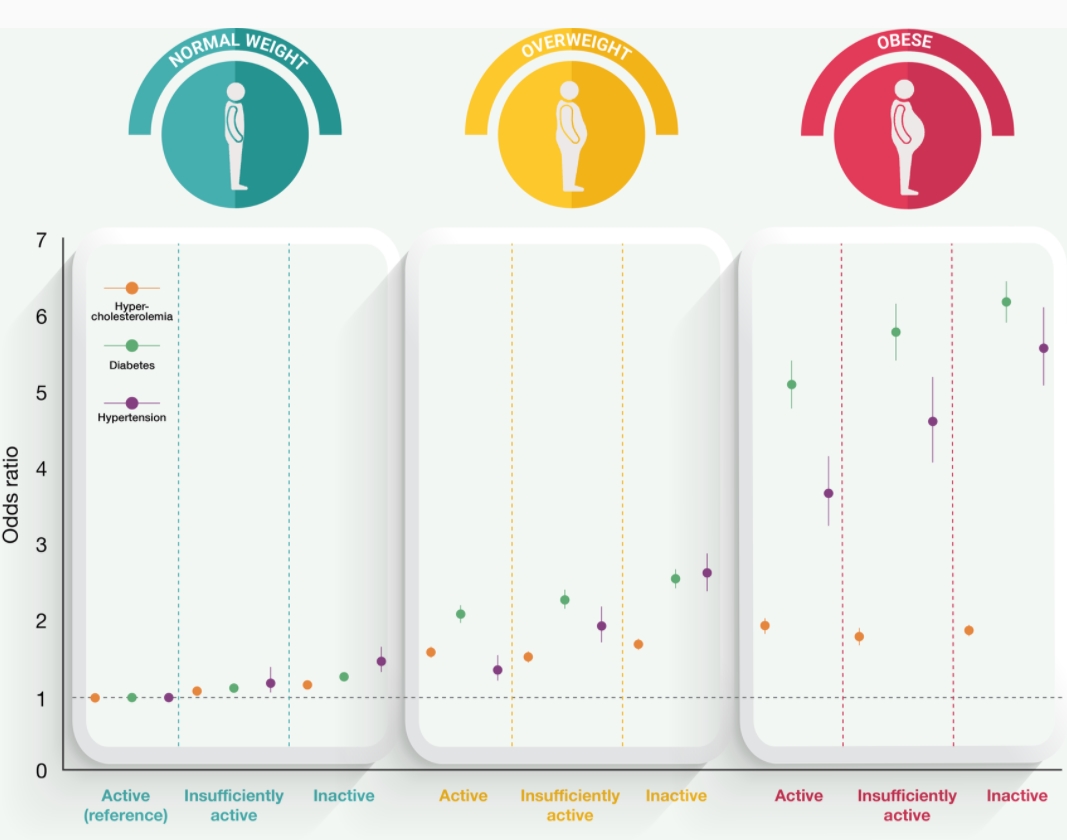
To clarify the existence of the ‘fat but fit’ [or ‘elevated body mass index (BMI) but active’] paradox, in this observational study, we assessed the joint association between different BMI categories and PA levels, respectively, and the prevalence of major CVD risk factors.
Participants (18–64 years, all insured by a large occupational risk prevention company) provided oral consent and the local ethics committee (reference#CEIC_2019_001) approved the protocol, which conformed to the Helsinki Declaration. Participants underwent routine medical examinations (∼1/year) as part of their health insurance coverage. The data obtained by the physician-directed examinations (2012–16) were collected during the last available examination.
Our study suggests that, although PA mitigates—at least partly—the detrimental effects of overweight/obesity on CVD risk, excess body weight per se is associated with a remarkable increase in the prevalence of major risk factors, as reflected by approximately two-, five-, and four-fold higher odds for hypercholesterolaemia, hypertension, and diabetes among active but obese individuals compared with their inactive peers with normal weight.
While the health benefits of increasing PA and maintaining an optimal body weight are widely known,5 whether the cardioprotective role of PA can counteract the detrimental effects of obesity remains controversial. In a recent prospective study involving 5344 adults, individuals with overweight/obesity who were physically active showed a similar risk of CVD events in a 15-year follow-up than their physically active peers with normal weight.6 A recent study involving 22 476 participants concluded that PA was associated with a larger reduction in the odds of 10-year CVD risk than having a normal weight.7 However, in line with our findings, a systematic review concluded that an excess BMI is associated with increased CVD risk irrespective of PA levels.8 Moreover, a study conducted in 2196 participants reported that although PA was associated with a lower CVD risk within each BMI category during a 30-year follow-up, individuals with overweight or obesity presented with an increased CVD risk regardless of their PA levels.9 Indeed, even ‘metabolically healthy’ obese individuals (i.e. those without cardiometabolic conditions, such as diabetes, hypertension, or hyperlipidaemia) present with a higher CVD risk than their peers with normal weight, as supported by a meta-analysis of 22 prospective studies.10 With the cross-sectional design we used, our analyses were not controlled for diet, and leisure-time PA levels were self-reported, representing potential study limitations. Nevertheless, the present findings, which are based on data from insured active workers across Spain, represent one of the largest studies to date (n = 527 662) and refute the notion that a physically active lifestyle can completely negate the deleterious effects of overweight/obesity.
In summary, increasing PA levels appear to provide benefits in an overall dose-response manner (regularly active > insufficiently active > inactive for the risk of hypertension or diabetes) across BMI categories and should be a priority of health policies. However, weight loss per se should remain a primary target for health policies aimed at reducing CVD risk in people with overweight/obesity.