Associations of vitamin K intake combined with vitamin D status with knee symptoms and structural changes in patients with knee osteoarthritis
Z. Liao Osteoarthritis and Cartilage VOLUME 28, SUPPLEMENT 1, S492, APRIL 01, 2020
Purpose: Vitamin D and K are both fat-soluble vitamins which are beneficial for bone metabolism. Vitamin D has therapeutic potential for osteoarthritis, and vitamin K is associated with prevalence or progression with OA. This study aims to investigate the association between vitamin K intake combined with vitamin D status and changes in knee symptoms and MRI structural features in knee OA patients over 2 years.
Methods: The parent study, Vitamin D Effect on Osteoarthritis (VIDEO) study, was a randomized, double-blind, placebo-controlled trial, which was conducted between June 2010 and December 2013 in Tasmania and Victoria, Australia. Participants with symptomatic knee OA and low 25-hydroxyvitamin D (12.5-60 nmol/L) were enrolled and randomly assigned to receive monthly treatment with oral 50000 IU vitamin D3 or an identical placebo for 2 years. Knee symptoms were assessed using the Western Ontario and McMaster University Index of osteoarthritis (WOMAC) score questionnaire. Serum 25(OH)-D was measured at baseline utilizing direct competitive chemiluminescent immunoassays (DiaSorin Inc.). A Food Frequency Questionnaire (FFQ), developing by the Cancer Council Victoria in Australia, was completed at baseline. Food vitamin K intake was calculated by multiplying the frequency of consumption of each food by the vitamin K content then adding the vitamin K content of all reported foods. Serum 25(OH)-D levels of ≤50 nmol/l was defined as vitamin D deficient, and of >50 nmol/l defined as vitamin D sufficient. Vitamin K intake status was classified as high (≥112 μg/d) and low vitamin K intake (<112 μg/d) based on the median. MRI scans of the study knee were obtained according to a standardized protocol using a 1.5 T whole-body MRI unit. Cartilage volume, cartilage defects, bone marrow lesions and effusion volume were measured at baseline and 24 months. We considered the lower vitamin K intake combined with vitamin D deficient as reference, then compared associations between different vitamin K intake combined with vitamin D status and changes in clinical or MRI features over 24 months using regression analyses. Stata version 14.0 was used to perform statistical analyses.
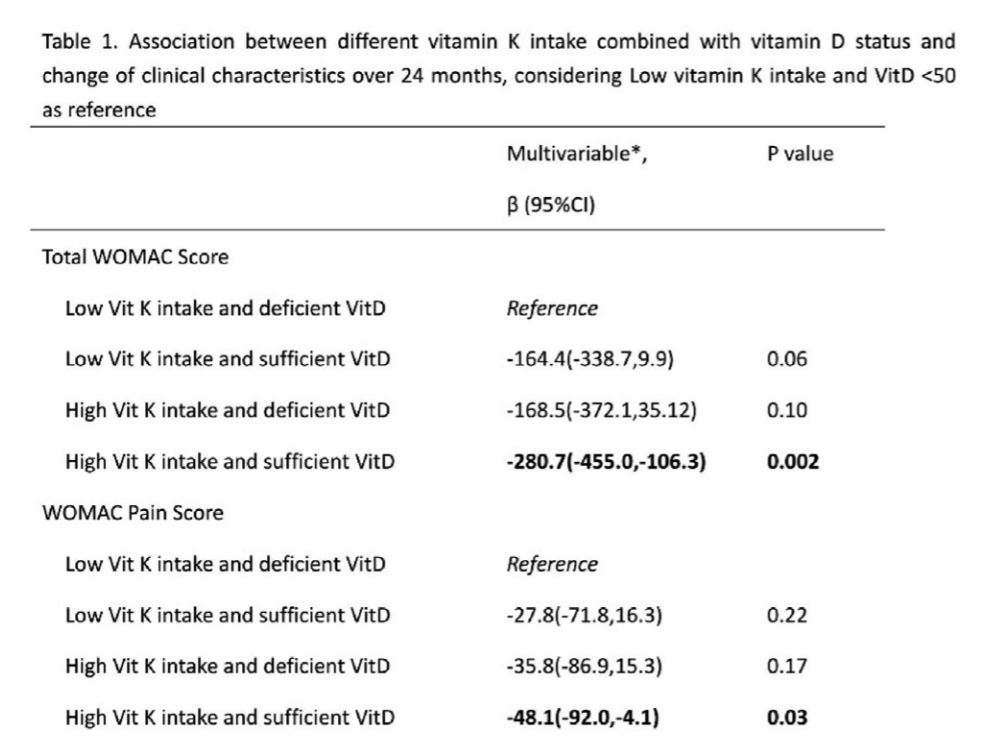
Results: Totally 261 participants in Tasmanian site were included at baseline and 213 completed the 2 years’ study. No significant difference for the baseline characteristics, including WOMAC scores and MRI features, was observed among different vitamin D combined with K status. Over 24 months follow-up, participants with high vitamin K intake combined with sufficient vitamin D had the most and significant improvement for total WOMAC Score, WOMAC Pain Score and WOMAC function score, compared to patients with low vitamin K intake combined with deficient vitamin D (Table 1). They also had the most but not significant improvement for WOMAC stiffness score. The participants with either high vitamin K intake or sufficient vitamin D also had more improvement for all four WOMAC score, compared to patients with low vitamin K intake combined with deficient vitamin D, but the differences were not significant. In contrast, no significant associations between different vitamin K intake combined with vitamin D status and changes in knee structures (cartilage volume, cartilage defect, bone marrow lesion, effusion) were observed.
Conclusions: High vitamin K intake combined with sufficient vitamin D status was associated with improvements in knee symptoms in patient with knee OA. This suggests possible synergistic effects of vitamin K and vitamin D on symptoms in knee OA.