Vitamin D and cardiovascular health
Fernando de la Guía-Galipienso Clin Nutr VOLUME 40, ISSUE 5, P2946-2957, MAY 01, 2021
The principal source of vitamin D in humans is its biosynthesis in the skin through a chemical reaction dependent on sun exposure. In lesser amounts, the vitamin can be obtained from the diet, mostly from fatty fish, fish liver oil and mushrooms. Individuals with vitamin D deficiency, defined as a serum level of 25 hydroxyvitamin D < 20 ng/dl, should be supplemented. Vitamin D deficiency is a prevalent global problem caused mainly by low exposure to sunlight. The main role of 1,25 dihydroxyvitamin D is the maintenance of calcium and phosphorus homeostasis.
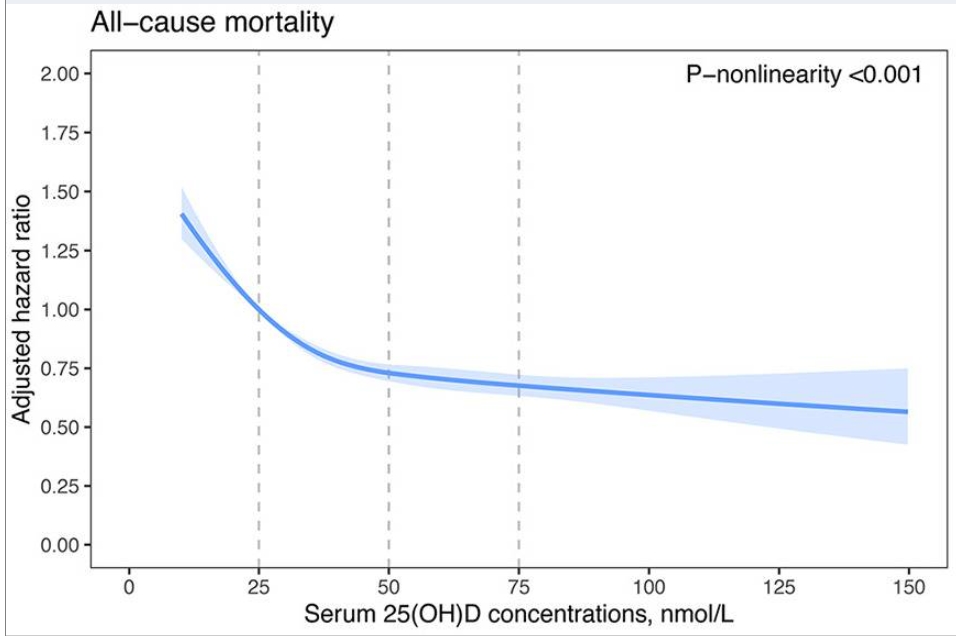
However, vitamin D receptors are found in most human cells and tissues, indicating many extra-skeletal effects of the vitamin, particularly in the immune and cardiovascular (CV) systems. Vitamin D regulates blood pressure by acting on endothelial cells and smooth muscle cells. Its deficiency has been associated with various CV risk factors and appears to be linked to a higher mortality and incidence of CV disease (CVD). Several mechanisms have been proposed relating vitamin D deficiency to CV risk factors such as renin-angiotensin-aldosterone system activation, abnormal nitric oxide regulation, oxidative stress or altered inflammatory pathways. However, in the latest randomized controlled trials no benefits of vitamin D supplementation for CVD have been confirmed. Although more work is needed to establish the protective role of vitamin D in this setting, according to current evidences vitamin D supplements should not be recommended for CVD prevention.