UEFA expert group statement on nutrition in elite football. Current evidence to inform practical recommendations and guide future researchJames Collins Br J Sports Med 2020
Football is a global game which is constantly evolving, showing substantial increases in physical and technical demands.
Nutrition plays a valuable integrated role in optimising performance of elite players during training and match-play, and maintaining their overall health throughout the season. An evidence-based approach to nutrition emphasising,
a ‘food first’ philosophy (ie, food over supplements), is fundamental to ensure effective player support. This requires relevant scientific evidence to be applied according to the constraints of what is practical and feasible in the football setting. The
science underpinning sports nutrition is evolving fast, and practitioners must be alert to new developments. In response to these developments, the Union of European Football Associations (UEFA) has gathered experts in applied sports nutrition research as well as practitioners working with elite football clubs and national associations/federations to issue an expert statement on a range of topics relevant to elite football nutrition: (1) match day nutrition, (2) training day nutrition, (3) body composition, (4) stressful environments and travel, (5) cultural diversity and dietary considerations, (6) dietary supplements, (7) rehabilitation, (8) referees and (9) junior high-level players. The expert group provide a narrative synthesis of the scientific background relating to these topics based on their knowledge and experience of the scientific research literature, as well as practical experience of applying knowledge within an elite sports setting. Our intention is to provide readers with content to help drive their own practical recommendations. In addition, to provide guidance to applied researchers where to focus future efforts.
View Full Text:
http://dx.doi.org/10.1136/bjsports-2019-101961UEFA expert group statement on nutrition in elite football: executive summary
Football (soccer) is a global game which is constantly evolving with substantially increasing physical and technical demands of match play. Training regimens have become more demanding physically, in an attempt to prepare players to cope with these evolutions and to address individual player needs.
Nutrition can play a valuable role in optimising the physical and mental performance of elite players during training and match-play, and in maintaining their overall health throughout a long season.Good nutrition choices can support the health and performance of footballers: the type, quantity and timing of food, fluids and supplements consumed can influence players’ performance and recovery during and between matches.1 2 However, the rapid evolution of the game itself, in addition to changes in our understanding of sports nutrition, has created uncertainty as to the appropriate nutritional decisions to make at specific moments in time and in specific contexts. In 2017, the steering committee of the current UEFA nutrition expert statement (JC, RM, JB, AMcC) committed3 to undertake an expert-led statement to update the knowledge and research about nutrition in elite football. We highlighted that the last expert-led statement on elite football nutrition had been written 11 years earlier.
While sports nutrition research since the last expert statement1 has in some instances helped to advance our knowledge and shape our practical strategies with elite footballers, the influx of new research brings with it confusion as to the relevance and veracity of current advice. It is often difficult for practitioners to interpret the available evidence and make sense of the controversies that may exist, in particular with the influx of different and opposing messages, especially from social media channels.4 In these instances, expert-led statements can be a powerful tool to aid practitioners with clarity on current research evidence.
This executive summary of the full scientific article—the ‘UEFA expert group statement’—provides a series of infographics illustrating important practical applications and insights that are intended to help practitioners take away some key points from the full article. We strongly advise practitioners to read and digest the full article and not only the practical infographic summary. This will ensure a more in-depth appreciation of the scientific evidence and the critical appraisals from the many experts involved which accompany the recommendations, in addition to understanding the fuller context and how to apply in their own practice.
In this expert group statement, nine specific topics have been identified: (1) match day (MD) nutrition, (2) training day nutrition, (3) body composition, (4) stressful environments and travel, (5) cultural diversity and dietary considerations, (6) dietary supplements, (7) rehabilitation, (8) referees and (9) junior high-level players. Our narrative synthesis and critical appraisal takes into account the diversity of the footballing community, including both male and female players, outfield players and goalkeepers and match officials.
As part of this process, UEFA has consulted with many specialists from the game to provide insights on the current role and future direction of nutrition in football. We often hear from the scientific community of the importance of sports science within football, but too often the voices of coaches are not heard in best practice guidelines, when they could offer valuable insight. Part of this executive summary includes an editorial by one of the world’s most iconic coaches, Arsène Wenger, who discusses the coach’s perspective on nutrition within the current footballing landscape and looks to the future of nutrition for players and teams around the world. We also have a brief ‘warm up’ to this UEFA expert statement from Marc Vouillamoz, UEFA Head of Medical and Antidoping and an editorial from Dr Tim Meyer, Chairman of the UEFA Medical Committee: these provide important antidoping and medical perspectives on the importance of nutrition in football.
As you will read in the full article and is evident throughout the series of infographics, the UEFA expert statement advocates an evidence-based approach to nutrition, and emphasises a ‘food first’ philosophy (ie, prioritising food over supplements to meet nutrient requirements) as being fundamental to ensure effective player support. It is crucial that clubs and national associations, where possible, use the services of qualified professionals with nutrition-related undergraduate degrees, postgraduate qualifications in sport and exercise nutrition and professional registration (depending on the country).
The expert statement process was created by a steering committee (JC, RJM, JB, AMcC) who identified the topics to be included and compiled a list of research and field-based experts. Expert group members (n=31 in total) included basic and applied researchers (n=6) and field-based practitioners (n=5); the majority (n=14) had a background of both research and field-based practice and six were UEFA Medical Committee members. It is intended that this narrative synthesis will provide readers with the scientific underpinning to inform their practical recommendations and strategies. In addition, we aim to guide applied researchers to focus their future efforts in regards to elite football nutrition research.
Introduction
Good nutrition choices can support the health and performance of footballers: the type, quantity and timing of food, fluids and supplements consumed can influence players’ performance and recovery during and between matches.1 2 However, the rapid evolution of the game itself, in addition to changes in our understanding of sports nutrition, creates uncertainty as to the appropriate nutritional decisions to make at specific moments in time and in specific contexts.
The physical and technical demands of elite football have increased in recent years,5 6 as have the financial implications of winning or losing. Training regimens have been adapted accordingly; they are more demanding and more sophisticated as they prepare players to cope with the evolution in match demands. Congested match schedules have been suggested to increase the risk of injury to players.7 8 Kick-off times have become more variable, with teams required to play early or late to accommodate television schedules. The travel required to compete in multiple domestic and international tournaments adds to the demands on players, with different logistical challenges depending on the geographical location. The reality being that the best players play the most often. Moreover, football truly is a global game9: frequent intracontinental and intercontinental matches and the migration of foreign players both result in greater cultural diversity and associated nutritional considerations.
The exponential rise in sports nutrition research in recent years has advanced our knowledge and expertise, but brings with it confusion as to what is actually sound advice. Those providing sports science support at elite level should follow an evidence-based approach,10 but it is often difficult for practitioners to interpret the available evidence and make sense of the controversies that may exist in particular with the influx of noise (ie, flawed messages) from social media channels.4 This, in part, reflects the limitations of our current knowledge:
we know, for example, that the recommended dietary allowance (RDA) is the average daily dietary intake that suffices to meet the nutrient requirements of nearly all (98%) healthy people, but it is unclear how these values should be applied in the assessment of dietary intakes of footballers and other athletic populations. We should also recognise that
much of the available data on dietary intakes is flawed, and probably does not reflect the true nutrient and energy intake of the populations that have been studied.11 Expert-led statements can be a powerful tool to aid practitioners in these instances, but although there are recent examples in different sporting situations,2 12 the most recent example of this in football-specific nutrition was a consensus published over a decade ago.1
The aim of this paper is to provide a narrative synthesis of the current evidence relating to various topics in elite football nutrition and in doing so, this manuscript is targeted at researchers, scientists and practitioners with scientific knowledge and understanding.
This UEFA expert group statement endorses and supports a ‘food first’ philosophy. This aims to establish best practice recommendations and represents an important next step in supporting the growth of nutrition within football. It is crucial that clubs and national associations, where possible, use the services of qualified professionals with nutrition-related undergraduate degrees, postgraduate qualifications in sport and exercise nutrition and professional registration (depending on the country); for simplicity, we use the term ‘sports nutritionist’ throughout.
We note several limitations to the evidence base from which recommendations of best practice can be reached:
There is little research specific to football, and the laboratory models that have been developed to simulate the game generally fail to replicate the demands of match play. As such, results need to be extrapolated from different sports and simpler exercise protocols.
Those studies that have used football as a model have been done with players engaged at recreational level. There is very little information derived from studies of elite players.
Many of the methods that have been used to assess the dietary habits of players and their nutritional status are fundamentally flawed and do not provide reliable information.
As with all studies, publication bias can increase the risk of a skewed picture of the efficacy of nutrition interventions, especially those involving the use of supplements. Studies that do not produce a positive outcome are less likely to be published than those that produce positive results.
We also recognise that, despite the great popularity of women’s football, there are few relevant studies. Nutritional needs and practices likely vary more within one sex than between sexes: the sex of the player is therefore another factor to be taken into account when considering the needs of an individual player.
Expert group statement process
A steering committee (JC, RJM, JB, AMcC) identified the topics to be included and compiled a list of research and field-based experts. Expert group members (n=31 in total) including basic and applied researchers (n=6) and field-based practitioners (n=5); the majority (n=14) had a background of both research and field-based practice and six were UEFA Medical Committee members. An outline of the expert group statement was agreed by all members: the authors were asked to focus on what is currently known from scientific research combined with their practical knowledge and expertise. First drafts of each section were collated by the steering committee to form the basis of the first full draft. This was circulated to all expert group members: the applied researchers focused on the narrative synthesis of the scientific research literature and the practitioners on the ecological validity in the football setting. Comments were collated and changes made before further review by the expert group. This process continued until agreement was reached on the specific sections and recommendations included (the whole process lasted from December 2017 to December 2019). A meeting between the steering committee and UEFA Medical Committee members (June 2019) was held to discuss and agree on any final amendments or additions that needed to be made and these were then circulated to the expert group for their review. This resulted in one further draft version before finalisation (December 2019).
The key recommendations are aimed at both male and female professional players, the majority of whom will be training and playing full time. Distinctions between male and female players are clearly made where appropriate; unless otherwise stated, the key recommendations apply to both sexes. Additional sections focus on elite referees and elite junior players (ie, players aged under 18 years and belonging to a professional football academy and training full-time).
Expert group topic 1: match day nutrition
Match play demandsDuring a football match, players engage in a variety of activities from walking to sprinting, changing direction, jumping and striking the ball, in addition to contact with opposition players. In outfield players, heart rate is maintained at an average of 85% of maximum and the average relative exercise intensity at 70% of maximal oxygen uptake (VO2max) over the duration of the match,13 equating to an energy expenditure of ~1300–1600 kcal,14 15 whereby carbohydrates (CHO) contribute about 60%–70% of the total energy supply.15 The total MD energy expenditure has been estimated at ~3500 kcal.16 To date, no studies have been performed to assess the physiological demands or fatigue responses of goalkeepers specifically.17 Limited research suggests that goalkeepers perform extended (~45–60 min) pre-match warm-ups and, while they cover less total distance and perform fewer high-intensity activities, they are rarely substituted and need to be prepared for a full 90–120 min match.17 The physical and technical demands of match play for elite outfield male footballers have increased substantially in recent years,5 6 likely as a result of tactical modifications.6
While the
total distance covered decreased by a trivial magnitude of 2% (10679±956 vs 10881±885 m) between 2006 and 2013, high-intensity and sprint running have increased substantially, with high-intensity running distance and high-intensity actions up by ~30% (890±299 vs 1151±337 m) and ~50% (118±36 vs 176±46), respectively.5 Over that same period of time, sprint distance and number of sprints rose by ~35% (232±114 vs 350±139 m) and ~85% (31±14 vs 57±20), respectively.
This trend is seen in all outfield positions (central defenders, full-backs, central midfielders, wide midfielders and attackers).5 Evolutions in technology have revealed that
players make more passes (35±17 vs 25±13), and that these are more successful (83%±10% vs 76±13%).5 These increased physical and potentially technically demanding (eg, cognitive) tasks make effective nutritional strategies even more important.Research on elite female players is sparse. The available evidence highlights that elite female players (international level)
cover approximately the same average total distance as their male counterparts, but they run less at high speeds.18 An important point to note is that no study has compared the high-speed or sprinting demands of male and female players relative to individual maximum speed. The use of absolute speed thresholds does not reflect differences in the maximum speed of individual players19 or gender differences.
Preparation for match play (carbohydrates and fluids)
CHO is the primary fuel for muscle during high-intensity activities; it is therefore a key macronutrient when preparing players for match play. On the day prior to a match (MD-1), training is usually light and CHO intake should be at least 6–8 g/kg body mass (BM) to elevate muscle and liver glycogen stores.20 While the glycogen cost of elite match play in either male or female players is not yet known,21 data from a friendly match involving lower division Danish male players demonstrate that approximately 50% of muscle fibres are classified as empty or partially empty after match play.22 Players who begin a game with low muscle glycogen stores will cover less distance and much less at high speed, particularly in the second half, than those who have ensured adequate glycogen stores.23 Where the match schedule consists of congested fixtures (eg, domestic fixtures, European competition, international games), CHO intake should be maintained within this range (6–8 g/kg BM/day) for the 48–72 hours between games to promote adequate glycogen storage. The reality is that
players often consume less than this and daily intake may be closer to about 4 g/kg BM.16 A conscious focus on the intake of CHO-rich foods is needed, with increased CHO intake at the cost of fat intake (and possibly protein intake) to ensure adequate glycogen restoration.Maintaining an appropriate hydration status will support players’ health and performance.24 Sweating is the primary mechanism to dissipate the metabolic heat generated during football training and match play in both cool and hot environments.25 26 Players should aim to start the match fully hydrated: daily BM measurements,27 degree of thirst,28 urine colour,29 osmolality and urine-specific gravity can be useful indicators of hydration status.30 A urine osmolality of <700 mOsmol/kg or a specific gravity of <1.020 suggests euhydration and >900 mOsmol/kg, hypohydration, although individual variability is present.31 For games with an early kick-off, the day prior to the match represents a key opportunity to optimise the players’ hydration status for the match the following day.
It has become popular in recent years to suggest that the only advice relating to hydration that is either necessary or appropriate for those involved in sport is to drink according to the dictates of thirst.32 This may not be appropriate in many team sport contexts, including football training and match play.33 The availability of fluids and the sensation of thirst may not coincide, and some forward planning (eg, understanding individual sweat losses, developing individualised hydration plans, alongside player education) can ensure that each player’s hydration needs are met.
Pre-match (CHO and fluids)On MD itself, CHO intake is again one of the most important considerations. Within an overall guideline of 6–8 g/kg BM CHO per day, it is recommended that players consume a CHO-rich meal (1–3 g/kg BM) 3–4 hours before kick-off to ensure that they begin the match with adequate glycogen stores. The pre-match meal is of particular importance for the promotion of liver glycogen stores, given that such stores can be reduced by about 50% after an overnight fast.34 This may be particularly important for matches with a lunchtime kick-off, and it highlights the importance of optimising nutritional preparation during the day prior to the match.
The pre-match meal should be easily digestible to reduce the risk of gastrointestinal problems (eg, reflux, discomfort). The pre-match meal should also make players ‘feel better’35 so comfort should be considered, rather than rigid strategies focused solely on meeting CHO intake guidelines. Player ‘rituals’ can be strongly held and education combined with practising pre-match fuelling in training or lower priority matches, can be an important tool to optimise glycogen stores and player readiness for match play.
Data from many studies suggest that high CHO intakes before and during a match can delay fatigue36 and enhance the capacity for intermittent high-intensity exercise.37 38 Benefits of pre-match meals may extend to players’ technical performance. For example, increased dribbling speed was observed when professional youth footballers consumed a larger breakfast (500 vs 250 kcal, with 60% CHO) 135 min before a match.39
Finally, players should aim to start the match euhydrated by ingesting 5–7 mL/kg BM of fluid in the 2–4 hours prior to kick-off.40 This allows time for excess fluid to be voided prior to exercise, targeting a urine that is pale yellow in colour.29
During match play (CHO and fluids)
Sufficient CHO and fluid intake are the two main nutritional considerations during match play.
Research evidence typically shows performance benefits in protocols simulating football matches when CHO is consumed during exercise at rates of ~30–60 g/hour,41–44 or when 60 g is consumed before each half.45 It is therefore recommended that ~
30–60 g CHO is consumed after warm-up and again at half-time to meet these guidelines. CHO ingestion during intermittent exercise also seems to improve shooting performance,38 46 dribbling speed,47 and passing,46 48 although the effects on sprinting, jumping, change of direction speed and cognition are less consistent.37 41 The current practices of elite players appear to be at the lower end of the ~30–60 g/hour scale; players in the English Premier League reported mean CHO intakes of 32 g/hour just before and during a match.16 This may be attributed to the match rules, which limit intake to warm-up and half-time (see below) and to the fear or actual experience of gastrointestinal problems during matches. This is a situation where sports foods (eg, CHO drinks, gels) can provide a preferred delivery option, to minimise these gastrointestinal issues. Stoppages during the match may also provide a valuable opportunity for players with increased CHO and/or fluid needs or for the whole team in hot conditions (see the section ‘Expert group topic 4’ on stressful environments).
Receptors in the oral cavity detect CHO consumed during exercise and exert central effects that may reduce the perception of effort.49 CHO mouth rinsing has been shown to increase self-selected jogging speed with likely benefits in sprint performance during intermittent exercise.50 The implications for football are still unclear,51 but the use of CHO mouth rinsing during breaks in match play (eg, half-time, extra-time, injury stoppages, medical breaks) could potentially enhance performance in situations where CHO consumption is limited by gastrointestinal concerns. On the other hand, it has been noted in recent tournaments that some players appear to misunderstand the mouth rinsing strategy and spit out the CHO-containing fluid even when there are no gastrointestinal problems. This may be partly due to the design of a scientific investigation in which there is an interest in distinguishing between the central nervous system and muscle fuel effects of CHO intake during exercise. Indeed,
swallowing the drink following a ~5 s exposure in the mouth allows both effects to occur simultaneously; this will be important in scenarios in which a player’s workload is high and CHO supplies may become limiting. It should be remembered that matches can extend to extra time and penalty shoot-outs where both the brain and muscle may benefit from additional fuel support and activation.
Sweat rates vary greatly between players and are primarily influenced by the intensity of exercise, environmental conditions and acclimation status.52 During training and matches sweat rates in male players have been reported to range from 0.5 to 2.5 L/hour26 53 54: lower values are generally reported in female players because of lower BM and lower absolute work rates.55–57
Sweat also contains electrolytes, primarily sodium, concentrations of which vary substantially between players.54 Mechanisms by which sweating-induced hypohydration might impair football performance are not completely elucidated, but may include increased cardiovascular strain,58 impaired cognitive function,59 increased perception of effort,60 reduced physical function60 and reduced technical skills.61 It is likely that individual players may be more or less sensitive to hypohydration during exercise. Therefore as a guide, players should aim to drink sufficient fluids to prevent a deficit of >2%–3% of pre-exercise BM during exercise,39 62 while avoiding gains in BM (hyperhydration) and also ensuring their fuel needs are met.38
Both hydration and CHO intake may require special attention in matches where extra time (2×15 min) is played. All match nutrition strategies, including the use of supplements (eg, sports foods), should be practised in training and minor matches to allow individualised protocols to be developed and to identify adverse effects in players, as well as allowing them the opportunity to become accustomed to any potential adverse effects, with minimal impact on important match performance.
Recovery from match play (CHO, fluids, protein)A primary objective following a competitive match is to reduce the time needed to fully recover.63 One essential goal is to rapidly replenish CHO stores. Postmatch meals and snacks should target a CHO intake of ~1 g/kg BM/hour for 4 hours.64 This is usually facilitated by the consumption of drinks and snacks in the changing rooms followed by post-match meals at the stadium, during travel and at home. Sports foods may provide a preferred option to supply macronutrients, especially to achieve CHO guidelines when appetite may be reduced or when sourcing food away from the home environment. Players should also aim to reduce any fluid and electrolyte deficit soon after the match65; however, in most situations there is sufficient opportunity and time to restore euhydration and electrolyte balance with normal eating/drinking practices, while also meeting other recovery objectives.63 65
Elite football players may not achieve CHO targets in recovery from evening games,66 suggesting suboptimal glycogen resynthesis patterns, the result of which is likely problematic for recovery and preparation during congested fixture schedules. As discussed above, daily CHO intake in the range of 6–8 g/kg BM in the 24 hours following a game (MD +1) will continue to replenish glycogen stores and this intake should be maintained for up to 48–72 hours after the match during congested fixture schedules. Higher intakes and additional nutritional strategies may be required when players report symptoms of muscle soreness and damage, as glycogen synthesis is impaired in the presence of muscle damage.67–69
To optimise protein synthesis for repair and adaptation, meals and snacks should be scheduled to achieve intakes of 20–25 g of (high-quality) protein at 3–4 hour intervals.70–72 Furthermore, there is emerging evidence that consuming 30–60 g of casein protein prior to sleep can enhance overnight protein synthesis.73Although postexercise protein intake undoubtedly increases protein synthetic rates and net protein accretion, this is a slow process and there is little evidence of acute improvements in muscle function.74 Some studies have reported reductions in muscle soreness with postexercise intake of protein or branched chain amino acids,75 but the overall effects are small. Consuming polyphenol-rich tart cherry juice has become a popular intervention to accelerate muscle recovery in different sports,76 77 but recent investigation in football did not show improved recovery markers of function or subjective soreness.78 Therefore, the available evidence does not support its specific use in football. Reducing exercise-induced muscle inflammation and free radical production, particularly with large doses of individual antioxidant vitamins C and E, may interfere with adaptive processes in muscle and is therefore discouraged.79
Alcohol
Some players may drink alcohol in social settings with teammates, friends and family, or as a means to relieve stress, anxiety or depression; this is particularly likely to occur after a match.63 Occasional intake of small amounts (no more than 2 units/day) of alcohol is not harmful, but alcohol use can interfere with recovery by impairing liver and glycogen resynthesis,80 muscle myofibrillar protein synthesis81 and rehydration.82 Drinking large doses of alcohol can also impair next-day countermovement jump performance83 and also directly suppress a wide range of immune responses84 and players should therefore minimise or avoid intake during key periods of training and match play when recovery is a priority.
Expert group topic 2: training day nutritionOverview of training calendar, objectives and training load
The football season is typically categorised into three distinct phases: preseason, in-season and off-season (see table 1). Despite more than four decades of research examining the physical demands of match play,6 85 86 detailed analysis of the customary training loads of elite footballers is comparatively recent and remains limited.20 87–89 These data demonstrate that training loads are lower than those experienced in match play, including total distance (<7 vs ~10–13 km),20 high-speed running distance (<300 vs >900 m),90 sprint distance (<150 vs >200 m)91 and average speed (<80 vs ~100–120 m/min).20 Absolute daily training loads depend on many factors including phase of the season,89 player position,89 coaching philosophy,88 89 frequency of games,92 player starting status88 and player-specific training goals such as manipulation of body composition93 or rehabilitation from injury.94
In the traditional in-season scenario of one match per week, players may complete four to five ‘on-field’ training sessions where the absolute training load is likely to be periodised across the weekly microcycle according to the proximity and importance of the game itself.20 Players may also undertake additional ‘off-field’ sessions, such as strength training. The aim is to stimulate both aerobic and strength adaptations while simultaneously rehearsing technical skills and tactics. It is noteworthy, however, that gym and field-based training sessions may not always be delivered in a systematic and structured sequence.95 The order of these can influence players’ habitual macronutrient intake and the magnitude of the strength adaptations induced.96 Both absolute daily intake and distribution of macronutrient intake have the capacity to affect training performance and recovery and to modulate training adaptations.
Carbohydrate requirements for training
Given the role of muscle and liver glycogen in supporting energy production during match play,22 it is important to consider their contribution to training goals. Unfortunately, the lack of specific data on muscle glycogen utilisation during typical field-based football training sessions makes it difficult to develop clear guidelines on the CHO requirements for training97 other than to suggest that they differ from the requirements for match play. Some information can be gleaned from the investigation of energy expenditure in English Premier League players during a 7-day in-season microcycle consisting of two games and five training days.16 The mean daily expenditure of outfield players was assessed at ~3500 kcal/day,16 with goalkeepers’ energy expenditure being ~600 kcal/day less.98 In these studies, the mean daily energy intake reported by players was comparable to energy expenditure, and BM did not change during the assessment period. Players reported an adjustment of daily CHO intake according to the perceived load, whereby ~4 and 6 g/kg BM were consumed on training and MDs, respectively. Nonetheless, given the importance of muscle glycogen for preparation and recovery from match play, it is suggested that players should increase CHO intake on MD-1, MD and MD +1 to between 6 and 8 g/kg BM. However, even at ~8 g/kg BM, muscle glycogen content in type II fibres may not be completely restored 48 hours after a match.99
Alternatively, given the lower absolute daily loads on typical training days (ie, one session per day in a one game per week microcycle) coupled with the fact that players typically do not perform any additional structured training outside of the club, daily intakes ranging from 3 to 6 g/kg BM may be sufficient to promote fuelling and recovery. In accordance with these lower absolute loads, it is unlikely that most players require CHO intake during training.16 However, this may depend on the duration and intensity of the training session, the timing of training in relation to the last meal and the potential benefits of practising CHO consumption during exercise to ‘train the gut’ to better absorb and tolerate intake during matches.
Daily CHO requirements for training should operate on a sliding scale of 3–8 g/kg BM/day depending on the specific training scenario, fixture schedule and player-specific training goals (further context is provided in table 1).
Protein recommendations for trainingDaily football training places stress on the musculoskeletal and tendinous tissues, and there is a need to remodel and repair these protein-containing structures to maintain and improve their integrity and function. Players may benefit from the provision of higher quantities of protein than are needed by the general population.
The RDA for protein is 0.8 g/kg BM/day in Europe,100 but higher intakes up to 1.6–2.2 g/kg BM/day appear to enhance training adaptation.101 Such levels of protein intake can easily be achieved from a mixed diet provided the energy intake is sufficient to meet the demands of training.102 Recent dietary surveys suggest that
most professional players report meeting or exceeding the 1.6–2.2 g/kg BM/day protein intake recommended for football. In professional players from the English Premier League, reported daily intakes of protein averaged 2–2.5 g/kg BM/day and were consistent across a 7-day in-season training period.16 This intake (approximately 200 g/day) was greater than that previously reported (<150 g/day) by adult players from the Scottish103 and Dutch104 leagues and is around twice the RDA in Europe, as previously highlighted. With judicious dietary planning,
protein supplements are probably not needed for most players, although they provide a convenient and easily digestible alternative to foods, especially in the post-training period. Where protein supplements are consumed at a dose of 0.3–0.4 g/kg BM/meal, whey protein is considered a prudent choice owing to its higher leucine content and digestibility.105
Ideally, three to four discrete protein-containing meals should be consumed each day, with at least ~0.4 g/kg BM/meal, which at four meals would provide ~1.6 g protein/kg BM/day.101 This strategy requires a plan to include protein-rich foods at each eating occasion to provide a sufficient dose to stimulate protein remodelling.
Protein quality may be important for players as the amino acid leucine, is an important trigger for muscle protein remodelling and ~2.5 g of leucine per meal would be optimal.105 Leucine content is highest in dairy-based proteins (2.5 g leucine/25 g serve of whey protein), high in meat (2.5 g leucine/140 g of lean beef or boneless chicken breast), eggs (2.5 g leucine/5 standard eggs) and plant-protein isolates like soya (2.5 g leucine/30 g serve of isolated soya protein).105
Plant-based proteins can also be used, but a higher protein intake is required for the same effect on muscle protein synthesis.105 As in the general population, football players often exhibit a skewed pattern of daily protein intake (the hierarchical order in which protein is consumed being dinner>lunch>breakfast>snacks), which while potentially meeting their daily protein intake (~1.6 g protein/kg BM/day) does not optimally stimulate protein synthesis on each meal occasion, although footballers are reported to consume ~0.3–0.4 g/kg BM at main meals,66 in line with current recommendations.
Emerging research on presleep protein consumption suggests that this is an important consideration for football players. Overnight is a natural regenerative phase and yet is also a time when nutrient intake is usually low or absent. Preliminary evidence supports
presleep protein ingestion106 107 at a dose of ~0.4 g/kg BM within 3 hours of bed in a full meal or perhaps 0.5 g/kg BM if consumed as supplemental protein 1–2 hours before bed to improve training adaptation during periods of high training volume.66 Professional players have typically reported an intake of only 0.1 g/kg BM at this time-point, highlighting an opportunity for improved nutritional choices that would potentially improve training adaptation.66During energy restriction, protein requirements are likely increased due to the catabolic milieu created by an energy deficit.108 109 Nonetheless, it is possible, even during a severe energy deficit, at least for athletes with high body fat, to lose fat and gain muscle simultaneously.108 For this reason, it is prudent to recommend a higher protein intake (perhaps 2.0–2.4 g/kg BM/day) that is dependent on training load and other metabolic stresses, such as weight loss or rehabilitation from injury (see the section ‘Expert group statement topic 7’ on nutrition for injury rehabilitation).94 110
Fat requirements for trainingDietary fat is an important part of a player’s training nutrition as an energy source, a vehicle for the intake and absorption of fat-soluble vitamins and a source of essential fatty acids. Adequate intakes of linoleic acid (an omega-6 fatty acid) and α-linolenic acid (an omega-3 fatty acid) typically provide ~10% of the overall dietary energy intake of sedentary people.111 Athletes are often advised to adjust fat intake to allow protein and CHO requirements to be met within total energy targets and to follow community guidelines regarding the minimal intake of trans fatty acids and caution with the intake of saturated fats. This typically leads to a fat intake of 20%–35% of total dietary energy. While some players may restrict fat intake to reduce total energy intake or because they think it is ‘healthy’, overrestricting fat intake to <15%–20% of energy often requires an unnecessary avoidance of a range of foods with valuable nutrient profiles. At the other end of the spectrum, there is renewed interest in chronic adaptation to a ketogenic low-CHO, high-fat (LCHF) diet to enhance the capacity for fat utilisation during exercise.112 Although there are anecdotal reports that some professional football players or teams follow such a diet (or a low-CHO (LC) diet), no observational or intervention studies involving team sports and LCHF diets are available. Furthermore, it has been shown that although trained muscle can use large amounts of fat at relatively high exercise intensities (eg, up to 75% VO2max) when CHO availability is limited, this is associated with an increased oxygen cost/reduced exercise economy which may at least partially explain the impairment of performance at higher exercise intensities.113 Due to the lack of evidence, an LCHF diet is not recommended for footballers.
Essential micronutrients for trainingFor elite footballers, the demands of both training and match play may also increase the requirements for some micronutrients to support metabolic processes within the body. There are many different classifications of micronutrients, including vitamins, minerals and trace elements essential for growth and development of the body. The most frequent cases of suboptimal status and key recommendations are outlined below.
Vitamin DVitamin D is a controversial topic in sports nutrition. Inadequate serum vitamin D concentrations have been reported to impair muscle function and recovery114 and to compromise immune health,115 so it is essential that football players who are deficient are identified and treated accordingly. It is a unique vitamin in that it can be synthesised in the skin via sunlight exposure, with <20% of daily needs typically coming from the diet.116 The average daily intake across the world is approximately 100–250 IU (1 ug = 40 IU), which is less than the current RDA of 400 IU (UK) and 600 IU (North America). The ability to synthesise vitamin D from sunlight is dependent on geography and meteorology, with UVB radiation being insufficient to convert 7-dehydrocholesterol in the skin to vitamin D at high latitudes, especially in the winter months. Paradoxically, studies demonstrate that,
compared with Caucasians, black and Hispanic people are at elevated risk of vitamin D deficiency (with darker skin colour reducing synthesis) but at lower risk of osteoporosis, rapid bone loss and associated fractures.116 Given that many footballers reside in countries far from the equator, and that many of them use sunscreen during the summer months, it is
not surprising that footballers117 occasionally present with vitamin D deficiencies. English Premier League football players showed a
seasonal pattern in vitamin D status, with 65% of players presenting with inadequate serum concentrations of 25(OH)D (25-hydroxy vitamin D, the best marker of vitamin D status) in the winter months.118
Low intakes have also been recorded in female players.119 120 The current target serum 25(OH)D concentration defined by the US Institute of Medicine and European Food Standards Agency is 50 nmol/L, although this may be conservative121 and it would be reasonable for athletes to aim for serum 25(OH)D concentrations of at least 75 nmol/L. There is emerging evidence that athletes can have too much supplemental vitamin D122; therefore, if a deficiency is observed, 2000 IU/day of vitamin D3 is suggested with retesting to confirm postsupplementation levels.
IronIron is the functional component of haemoglobin and myoglobin as well as being an essential constituent of non-haem sulphur enzymes and haem-containing cytochromes involved in oxidative ATP production. Therefore, iron deficiency, even without anaemia, can have negative implications for aerobic performance.123–125
Due to regular blood loss during menstrual bleeding (and possibly due to a diet less rich in meat), postpubertal female players are at the highest risk of iron deficiency.126 127
While iron deficiency in athletes is common, with a prevalence of about 15%–35% in female athletes and 5%–11% in male athletes,128 data on professional football players at various stages of the season are limited. Iron deficiencies may present as lethargy and reduced performance and can be identified through blood screening. A reasonable time frame for assessment of iron status is once per year in male players and twice per year in female players (more frequently when iron deficiency has been detected in recent monitoring).
Anaemia is considered present when blood haemoglobin levels are <115 g/L (females) or <125 g/L (males), although some laboratories may use slightly different cut-off values. Iron deficiency is defined as low serum ferritin (<35 µg/L) and normal (ie, not yet affected) blood haemoglobin values. In young athletes, iron deficiency represents the most frequent cause for anaemia; it is typically tested for by determining serum ferritin, the most established marker for the amount of stored iron.129 130 Anaemia in the presence of low serum ferritin indicates that the anaemia is due to iron deficiency. For anaemia with regular ferritin values, it is necessary to consider other possible causes. In the cases of iron deficiency anaemia, there is a need for iron substitution. When only ferritin is lower than normal, a diet rich in iron, particularly red meat, is recommended to avoid the development of overt anaemia and make sure that other haem-containing proteins/enzymes can be maintained at a sufficient level. Additionally, a period of iron supplementation may be considered at levels above the RDA after consultation with qualified medical and dietetic practitioners. Parenteral (ie, intravenous) supplementation is usually not indicated. Only in cases of pathologically impaired iron digestion from the gut (such as in coeliac disease) is an intravenous administration justified, also with further consideration of maximum infusion volumes outlined by the most recent antidoping regulations. Determination of transferrin saturation can be an alternative means of assessing iron status when ferritin is not available.130 This sometimes occurs when an infection or inflammation is present at the same time because ferritin is an acute-phase protein and typically increases slightly during such episodes.
Low iron status may result from red cell haemolysis, gastrointestinal bleeding, sweating, inflammation, menstruation in female players and inadequate dietary intake.131 132 The bioavailability of dietary iron is substantially lower in vegetarian diets than meat-based diets, so the growing interest in veganism is a concern with regard to dietary iron content. The current RDA for iron is 18 mg (in North America) or 14.8 mg (in the UK) for females, and 8 mg (North America) or 8.7 mg (UK) for males. Where possible, iron should be consumed from highly bioavailable sources (haem iron), including meat and seafood. Vitamin C should be co-ingested with non-haem iron sources to enhance absorption, and foods or fluids that impair iron absorption, such as tea and coffee, should be avoided around meal times. Numerous oral iron preparations are available, and most are equally effective if appropriately taken. Gastrointestinal side effects of supplementation can include constipation, nausea and black stools. The tolerable upper intake level (UL) is 45 mg/day; high-dose iron supplements of >45 mg/day elemental iron should not be taken unless iron deficiency is present, as there is a real danger of harmful iron toxicity. For further information on iron considerations, readers are directed to a review by Sim et al.128
CalciumCalcium is important for the maintenance of bone tissues, skeletal muscle and cardiac contraction and nerve conduction. Serum calcium concentration is tightly regulated by calcitonin and parathyroid hormone regardless of acute calcium intake. The largest store of calcium in the body is in the skeleton and this store is mobilised when dietary intake is inadequate, leading to demineralisation of bone tissue through the action of parathyroid hormone. Dairy products are the main dietary sources of calcium, but it is also found in green leafy vegetables, nuts and soya beans (table 2) The RDA for calcium is 1000 mg/day (North America) or 700 mg/day (UK) for adults and 1300 mg/day (North America) or 1000 mg/day (UK) for adolescents. An athlete’s diet should include a higher intake of 1500 mg/day through dietary sources or supplementation if required to optimise bone health in cases of relative energy deficiency in sport (RED-S).133 Calcium may be lost through sweat, although modestly; this can hypothetically reduce serum ionised calcium concentration, resulting in an increase in parathyroid hormone production, thus stimulating bone resorption.134 Significant dermal calcium losses have been reported following prolonged exercise alongside an increase in parathyroid hormone.135 In support of this hypothesis,
ingestion of 1350 mg of calcium 90 min prior to exercise has been shown to attenuate deleterious changes in biomarkers of bone resorption.136 This suggests that
dermal sweat losses, as well as urinary losses,137 although small, may be an important consideration. Particular attention should therefore be given to football players training or competing in hot environments, especially if they have low dietary calcium intakes. If supplements are to be used,
calcium carbonate and calcium citrate are well absorbed. Finally, recent research has highlighted that
magnesium is an emerging consideration with its role in energy production, muscle function, bone heath, immune function and pain modulation. A recent
8-year study in Olympic athletes highlighted 22% of athletes were deficient (estimated from erythrocyte magnesium concentration) at one time-point. Furthermore,
athletes with a history of Achilles or patella tendon pain had significantly lower magnesium levels than average.138


 Forum Nutrimuscle, Nutrition, musculation, transparence !
Forum Nutrimuscle, Nutrition, musculation, transparence !  Actualités, vidéos, études scientifiques
Actualités, vidéos, études scientifiques
![]() par Nutrimuscle-Conseils » 30 Oct 2020 12:49
par Nutrimuscle-Conseils » 30 Oct 2020 12:49 ![]() par Nutrimuscle-Conseils » 30 Oct 2020 12:51
par Nutrimuscle-Conseils » 30 Oct 2020 12:51 ![]() par Nutrimuscle-Conseils » 30 Oct 2020 12:52
par Nutrimuscle-Conseils » 30 Oct 2020 12:52 ![]() par Nutrimuscle-Conseils » 30 Oct 2020 13:26
par Nutrimuscle-Conseils » 30 Oct 2020 13:26 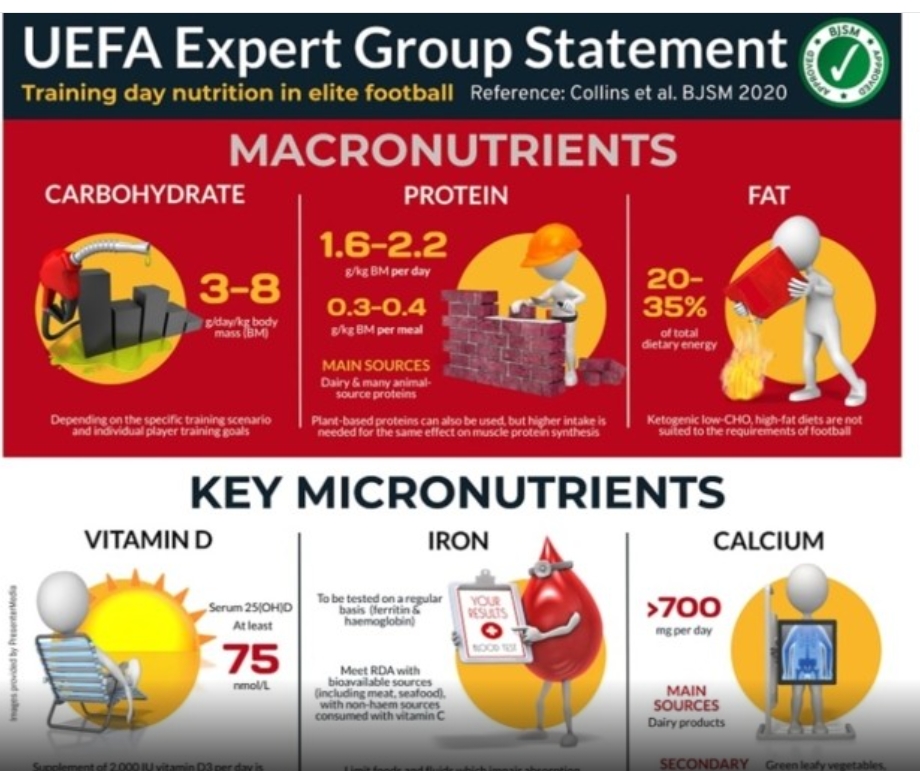
![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:43
par Nutrimuscle-Diététique » 30 Oct 2020 18:43 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:45
par Nutrimuscle-Diététique » 30 Oct 2020 18:45 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:46
par Nutrimuscle-Diététique » 30 Oct 2020 18:46 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:47
par Nutrimuscle-Diététique » 30 Oct 2020 18:47 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:48
par Nutrimuscle-Diététique » 30 Oct 2020 18:48 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:48
par Nutrimuscle-Diététique » 30 Oct 2020 18:48 ![]() par Nutrimuscle-Diététique » 30 Oct 2020 18:49
par Nutrimuscle-Diététique » 30 Oct 2020 18:49 ![]() par Nutrimuscle-Conseils » 10 Déc 2020 10:34
par Nutrimuscle-Conseils » 10 Déc 2020 10:34 ![]() par Nutrimuscle-Diététique » 10 Déc 2020 18:05
par Nutrimuscle-Diététique » 10 Déc 2020 18:05 ![]() par Nutrimuscle-Conseils » 12 Juin 2021 18:49
par Nutrimuscle-Conseils » 12 Juin 2021 18:49 ![]() par Nutrimuscle-Conseils » 16 Juin 2021 12:59
par Nutrimuscle-Conseils » 16 Juin 2021 12:59 










