Omega-3 fatty acids in the psychological and physiological resilience against COVID-19
Jane Pei-Chen Chang Prostaglandins, Leukotrienes and Essential Fatty Acids September 24, 2020
Highlights
• This is the first review on Omega-3 and COVID-19.
• Increased mood disorders during COVID-19.
• Omega-3 may improve COVID-19 associated mood symptoms via immunomodulation.
As the infected cases of COVID-19 reach more than 20 million with more than 778,000 deaths globally, an increase in psychiatric disorders including anxiety and depression has been reported. Scientists globally have been searching for novel therapies and vaccines to fight against COVID-19. Improving innate immunity has been suggested to block progression of COVID-19 at early stages, while omega-3 polyunsaturated fatty acids (n-3 PUFAs) have been shown to have immunomodulation effects. Moreover, n-3 PUFAs have also been shown to improve mood disorders, thus, future research is warranted to test if n-3 PUFAs may have the potential to improve our immunity to counteract both physical and mental impact of COVID-19.
1. Introduction
Omega-3 polyunsaturated fatty acids (n-3 PUFAs), including docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), are essential fatty acids for our brain and immune system, and can only be obtained from diet. There have been several studies showing that deficiency of n-3 PUFAs have been associated with several psychiatric disorders including major depressive disorder (MDD) [1], perinatal depression [2], attention deficit hyperactivity disorder (ADHD) [3], and dementia [4]. On the other hand, interventional studies with n-3 PUFAs supplementation have been show potential to improve the clinical outcome of MDD [5], perinatal depression [6], ADHD [7], anxiety disorder [8] and mild cognitive impairment [9]; and even prevent interferon-induced depression [10]. Moreover, a recent practice guideline on n-3 PUFAs on MDD has also been published by the International Society for Nutritional Psychiatry Research (ISNPR) [11]. The guideline suggested a clinical interview is recommended to validate the clinical diagnoses prior to the prescription of n-3 PUFAs, the ratio of EPA/DHA in the formula should be greater than 2, and the dosage should be 1-2 g of net EPA. The guideline further emphasized that quality of the supplementation will affect the therapeutic activity and that potential adverse effects such as gastrointestinal and dermatological conditions should be closely monitored along with metabolic profiles. Thus, in the current Pandemic, n-3 PUFAs may perhaps serve as a potential nutraceutical to prevent COVID-19 associated neuropsychiatric sequelae such as depression and anxiety or the relapse of MDE in those with pre-pandemic MDD.
2. COVID-19 and Psychiatric Disorders
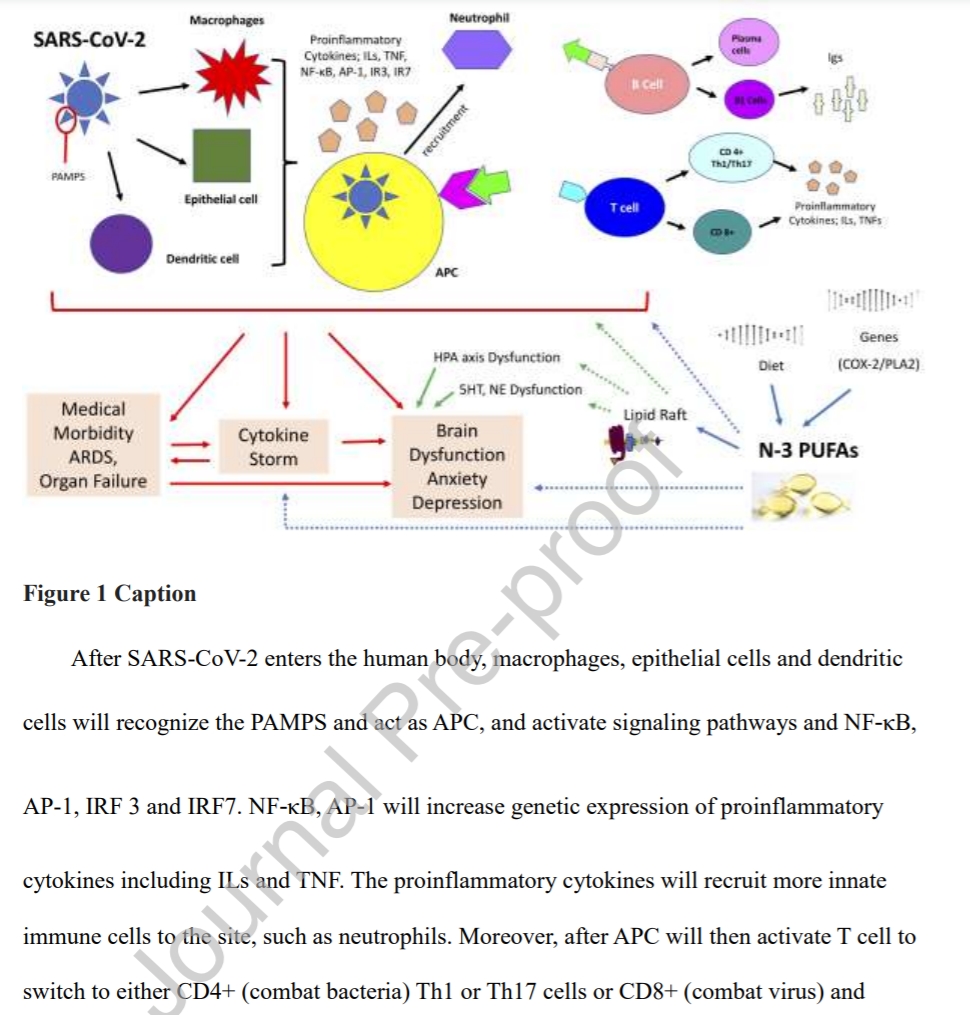
COVID-19, up until now, has infected more than 20 million people and took 778,219 lives globally (18th of August, 2020) (https://www.worldometers.info/coronavirus/). Individuals of older age, smoking habits, chronic medical conditions, and immunocompromised status are more susceptible for contracting COVID-19 and resulting in fatal complications [12]. Moreover, those who survived the Pandemic, regardless COVID-19 infection, may have an increase in anxiety and mood disorders [13]. This brief review aims to discuss the potential role and application of n-3 PUFAs in fighting against COVID-19 both mentally and physically via immunomodulation [14] (Fig. 1).
3. COVID-19, Immune Reactions, Mood Disorders
The first two weeks after infection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV2, the virus causing COVID-19) are crucial. Whether the patient will develop serious complications such as acute respiratory distress syndrome (ARDS) or other organ failure depends on the individual's innate immunity and the exposure to the viral load [15]. If the virus is successfully blocked at the upper airway and does not reach the lungs, then the individual has a greater chance of having a milder form of COVID-19 [15]. However, if the SARS-Cov-2 do reach alveoli, it will have more replications, active the specific adaptive immune response. This may result in interleukin (IL)-6 cytokine storm and disseminated intravascular coagulation (DIC), both are common causes of death in COVID-19 infection [15]. On the other hand, IL-6 has been associated with mood disorders [16], and has been investigated as a potential treatment for mood disorders [5].
The innate immune system recognizes the pathogen‐associated molecular patterns (PAMPs) produced during SARS‐CoV‐2 infection, and will activate signaling pathways and transcription factors including nuclear factor κB (NF‐κB), activator protein 1 (AP‐1), interferon response factor 3 (IRF3), and IRF7. NF‐κB and AP‐1 will then induce genetic expression of proinflammatory cytokines including tumor necrosis factor (TNF) and IL‐1 and chemokines including CCL2 and CXCL8. However, the mechanism where interferon (IFN)‐α and IFN‐β are used to suppress viral replication at early stages appeared to be bypassed during SARS-Cov-2 infection, which may result in uncontrolled viral replication [17]. Thus, strengthening innate immunity is a crucial step to block the progression of COVID-19. Furthermore, the proinflammatory cytokines will recruit other innate immune cells including macrophages, neutrophils, and natural killer (NK) cells, and lead to the activation of adaptive immunity, where T helper (Th)1/Th17 cells may cause immunopathologic lung injury that leads to pneumonia [18]; while B cells may produce specific antibodies that may help neutralize SARS‐CoV‐2 [18]. In addition, impaired lymphocyte function has been suggested to contribute to the development of mood disorders [19], which has increased global incidence during the Pandemic [13].
4. N-3 PUFAs, Immune Reaction, Mood Disorders
N-3 PUFAs and its metabolites, pro-resolvin mediators (SPMs) including prostaglandins, leukotrienes, thromboxanes, maresins, protectins and resolvins (Fig. 1), have been shown to have immunomodulatory functions [20]. N-3 PUFAs help to modulate the migration, increase the phagocytotic capacity, decreases the cytokine production and the reactive oxidative species (ROS) of innate immune cells including macrophages and neutrophils [14]. Moreover, n-3 PUFAs and its metabolites also promote activation of NK cells and modulate the T cell activation by altering activation of antigen-presenting cells (APCs, such as macrophages or dendritic cells) and prevent the differentiation of CD4+ cells to Th1 cells [14]. In addition, n-3 PUFAs also increase innate-like B cells, B1 cells, and immunoglobulin (Ig)M production by B cells, by increasing the number of APCs [14], which may altogether strengthen the innate immunity. Moreover, n-3 PUFAs, especially EPA, have shown effect in treating mood disorders via reduction of pro-inflammatory cytokines, alteration of hypothalamus-pituitary-adrenal (HPA axis), and modulation of neurotransmission via lipid rafts [21]. (Fig. 1).
5. Potential Role of N-3 PUFAs in COVID-19
In sum, by strengthening baseline immunity may help prevent fatal outcomes and psychiatric sequelae in those individuals infected with COVID-19 or prevent the relapse of pre-pandemic psychiatric disorders. Thus, a healthy and balanced diet may be what we need to improve our immunity, and future research are warranted to test if n-3 PUFAs may be the potential nutraceutical to help maintain both our mental and physical wellbeing during this Pandemic.